- 11 Posts
- 3 Comments
Joined 2 years ago
Cake day: March 13th, 2023
You are not logged in. If you use a Fediverse account that is able to follow users, you can follow this user.
 0·8 months ago
0·8 months agoYou’d think so, wouldn’t you? People have been locked-away for treason after lesser acts than Jan 6. Treason laws in the United States . If the feds won’t prosecute, I’d hope the state AGs would start to look into these kind of public displays of insurrection.
 0·9 months ago
0·9 months ago(2019)








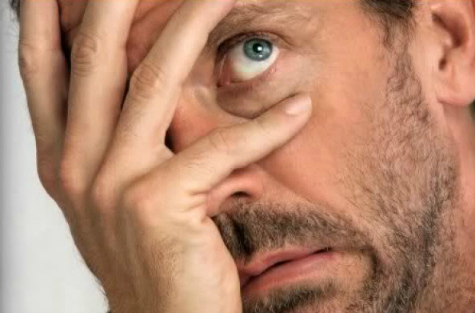
Yep. My criminal insurance company (CIC) marketing docs trumpeted how my ER costs were “fully covered” (which they’re required to be by law, I think). That’s obviously bad for profits, so the solution? Well just interpret any ER line-item (pick some expensive ones) as non-ER, even when they pertain to an ER visit, then charge the whole slew of separate copays/deductibles that go with the new interpretation. Profit! The hospital, which has a contract with the insurer, will cooperate and code all these line-item services with ambiguous language and codes, making them ripe for the picking by the screw-you insurance dweebs.
Oh, I can appeal the insurance decisions? Great. Appeal #1 is decided by the insurance company itself! 100% internal. Appeal #2 is done by a third party company, selected by the insurance company and paid by the insurance company. Think your state insurance commissioner is going to step in when foul play occurs? Think again. If they pay attention to you at all, they’ll claim to have no “authority” to make “medical decisions” about the abuse the insurance companies subject you to, and if they do anything at all, it might be to write a mildly-stern email to the insurance company reminding it of your complaint and their supposed obligations. That’s it, the commissioner’s office is not on “your side” and even if it were to some extent, they’ll claim to be “too overloaded” to do anything, anything like actually regulate the insurance companies, on your behalf or on behalf of the other millions of insurance customers.